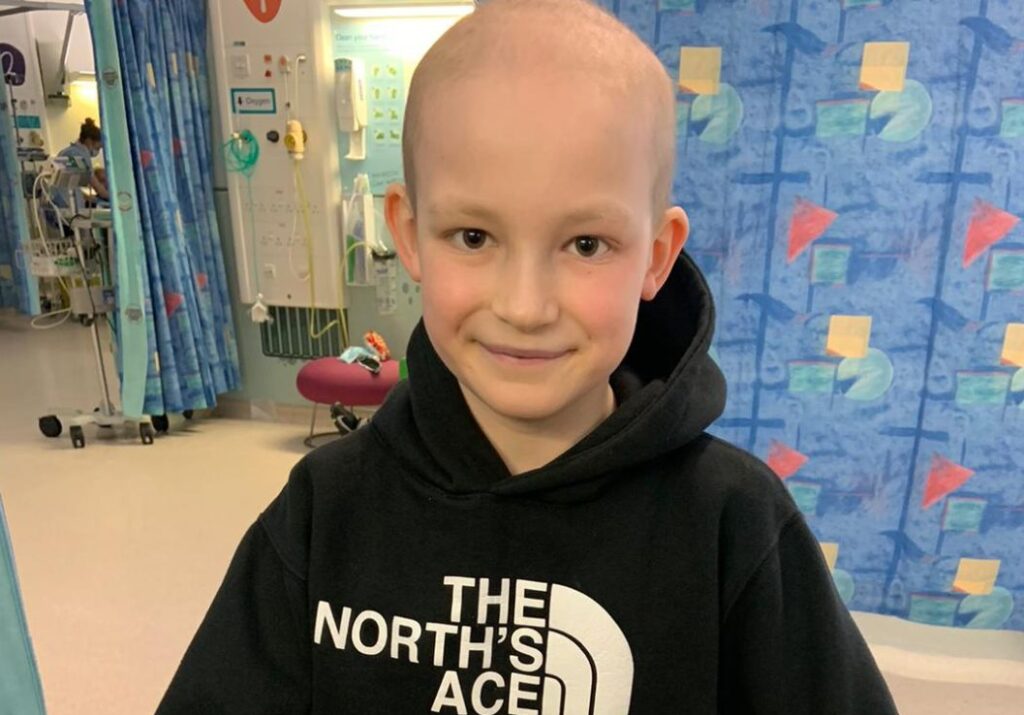
Austin, now 16, has spent nearly eight years fighting Acute Lymphoblastic Leukaemia (ALL). For many children, treatment for ALL lasts around three years with a high success rate. But Austin’s journey was far from typical. Multiple relapses, serious infections, and life-threatening complications meant his treatment stretched over seven years.
In 2011, two year old Austin fell ill. After several visits to the hospital and repeated diagnoses of tonsillitis, his parents insisted on a blood test. Just hours later, doctors delivered the devastating news, Austin had Acute Lymphoblastic Leukaemia.
His dad, Scott, recalls how things moved quickly “The very next day we were transferred from the local hospital to Royal Victoria Infirmary in Newcastle, where Austin would begin his treatment.” Unfortunately, within days, Austin contracted pseudomonas, a life-threatening bacterial infection. He spent three months in bed, endured skin grafts, a colostomy bag, and intensive care – before learning to walk again. This delay forced him onto a more aggressive treatment regimen, but still, he relapsed twice more.
Chemotherapy, radiotherapy, and even a bone marrow transplant from a generous donor in Germany – could not keep the disease away.
By late 2015, after his third relapse and a lung infection, doctors told the family there was nothing more they could do. Austin was brought home, and his family prepared for the worst. Louise remembers, “This was one of the darkest times we experienced as a family.” Miraculously, after a week, Austin began to recover. “Many said it was a miracle, but at just the last moment, he started producing neutrophils again.”
That’s when the family heard about a clinical trial at Great Ormond Street Hospital (GOSH). Meeting Professor Persis Amrolia was a turning point. Scott remembers that day clearly “He was talking about potential hope, and suddenly we could see a future – both for Austin, and for medicine.” The trial ‘CD-19 TPALL’ offered a revolutionary approach, CAR T-cell therapy, a form of personalised immunotherapy. Unlike chemotherapy or radiation, CAR T cells are programmed to target only cancer cells, sparing much of the healthy tissue.
Uprooting life to move from Whitley Bay to London for treatment was daunting, but it gave Austin his best chance. Scott explains, “It was a massive adjustment… But we did what we had to do.” In September 2016, Austin underwent CAR T-cell therapy. When those cells didn’t take, Persis offered an alternative version of the trial, CD-19 CART. Austin received these in October 2016 – and on his birthday, the family received the news they had hoped for, the cells were working.
Austin’s family knew they couldn’t put him through more of the same treatments that had failed before. Scott, a design and technology teacher, puts it into perspective.
Today, Austin is living with the long-term effects of his treatments, including reduced growth, cataracts, and learning challenges. But he’s thriving. He’s completed his GCSEs and works at the local ice cream shop. For Louise and Scott, parenting has returned slowly to something closer to normal. “We aren’t worrying all the time. And though we never thought it possible, we now go for long periods without thinking about his illness.”
Austin’s story is exactly why we need The ATICUS Network. This network would connect 11 specialist centres across the UK, ensuring that innovative trials like Austin’s are available wherever they are needed – faster, and for more children.
Thank you for reading Austin's Story
Read our inspiring patient stories

Christine’s Story

Steve’s Story

Alyssa’s Story
Hughie’s Story

Morgan’s Story

Kathryn’s Story

Elizabeth’s Story

Austin’s Story

Neil’s Story
