
Patient Case Study: Madeline Hawkins
Madeline Hawkins was diagnosed with Chronic Myeloid Leukaemia (CML) back in June 2012 after she was referred for additional blood tests following complains of pain in her feet.
Retired teacher Gerard Lancaster, from Stockport, is feeling fighting fit, despite being diagnosed with Ankylosing Spondylitis, Thyroid Cancer and eventually acute myeloid leukaemia (AML) over the past half century.
Gerard, 84, now is currently half-way through the second cycle of a clinical trial, recommended to him by staff from our Trials Acceleration Programme (TAP) Centre at The Christie NHS Foundation Trust in Manchester.
We are sharing Gerard’s story in his own words to mark KnowAML Day this week and to highlight the importance of clinical trials and why networks like the Cure Leukaemia funded TAP are so vital to give hope to the 38,000 people diagnosed with a form of blood cancer in the UK each year.
The discovery of my leukaemia, Acute Myeloid Leukaemia, was almost accidental – a result of several other medical conditions having to be checked.
I was born in 1936, so I am currently 84 years old. I am married to my wife, Dorothy, and I have one daughter who lives with her husband and two children near London.


Dorothy and I are both retired teachers – I retired in 1992 and Dorothy in 1993, so we’ve had a long retirement. I taught physics and other sciences and Dorothy was a junior school teacher.
Around the age of 30, I was diagnosed with ankylosing spondylitis (AS). This is still a poorly diagnosed condition, often being identified only after years of symptoms. In my case it was treated mainly with pain relief and I continued my life without any other intervention, but with a typical AS posture.
As teachers, with long summer breaks, we travelled – camping and then caravanning. After retirement I worked as a self-employed toy maker and repairer, mainly in local schools. Also, I walked every week with a group of other retired folk – initially 10 to 12 miles in the Peak District, but in recent years, as we all aged, only 6 or 7 miles and fewer hills.
When the pandemic appeared, the group stopped meeting, or walked in pairs and I didn’t take part – so I didn’t notice any consequences of my subsequently diagnosed AML.
In, I think 2012, I was found to have thyroid cancer.
It was treated quickly, initially at Stepping Hill Hospital, my local hospital and later at MRI in Manchester and later at The Christie.
The AS made the surgeon’s work more difficult. Half the thyroid was removed at MRI and the other half treated at The Christie with an iodine ablation. Over the intervening years I have had frequent consultations at The Christie but in the last few years I have just had blood tests and an annual review. There were no particular concerns.
.jpg)

Gerard with his grandchildren on his 80th Birthday
My own GP surgery always made a point of repeating the blood tests for their records.
For about 30 years I have had intermittent periods of stomach discomfort. There were investigations which didn’t find any serious concerns, and sometimes my posture, resulting from the ankylosing spondylitis, was seen as a contributory factor.
In January 2020 I had a telephone consultation with my GP about stomach pains and we decided it was a repeat of the same problem and medication was prescribed and the symptoms disappeared.
Then in mid-July the stomach symptoms re-appeared and I spoke to my GP again. Because of the pandemic, this year’s annual tests at The Christie had been replaced by a telephone consultation, and no blood tests. My GP suggested that I attend the surgery for a face-to-face consultation and they would do a blood test for their own records on the thyroid condition.
She phoned me when the blood test results came back – concerned about low values – and telling me to self-isolate or go into shielding.
.jpeg)
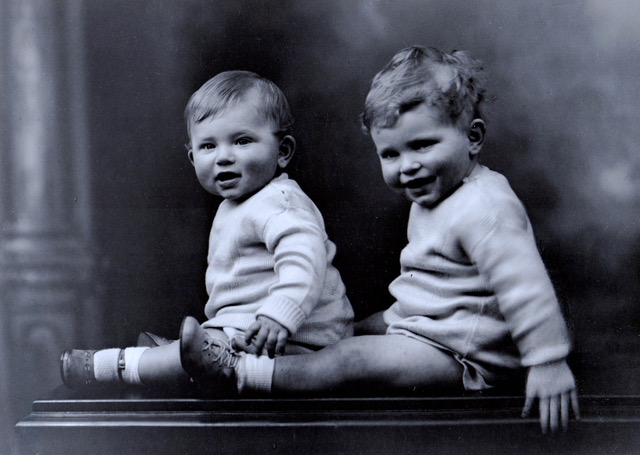
Gerard pictured with his brother Jim in the 1930s. Jim sadly passed away last year.
She also put me on a list for colonoscopy and for a scan of some sort, but also arranged further blood tests. A second and third set of bloods were taken over the next ten or so days.
Then she rang to say I had a very serious condition – don’t delay, pack a bag, collect a note from the surgery and go directly to A&E at the local hospital.
By the end of that day I had had blood tests, an ECG, a scan of some sort, an X-ray and been visited by increasingly senior staff.
I was told (very gently but definitely) that I had a form of leukaemia and that it was probably life threatening “perhaps you would like to inform local relatives?”
Over the next couple of days in the hospital I was given intravenous antibiotics and a blood transfusion and had a bone marrow biopsy.
The following week, early August, I had an appointment at The Christie which I attended with my wife. The consultant explained in some detail what my condition was and what the outlook was. At my age, a full-on course of chemotherapy was not considered sensible. Instead, a more palliative course of treatment, low-dose cytarabine, was recommended. There was some chance of remission, maybe 20%.
Again, my AS played a part – the low-dose cytarabine injections had to go under the skin on my stomach, but my AS-restricted movement meant I couldn’t bend far enough to actually see that bit of my body. Dorothy was ‘volunteered’ to do the injections.
After a couple of courses, there had been an improvement, from 80% leukaemia cells down to 40% – it sounded good to me, but it was described as ‘sub-optimal.’
I think that it was after a third course of low-dose cytarabine that the possibility of a different approach was suggested. The consultant offered the option of taking part in a trial of new drug and that’s where I am today, half-way through the second cycle of the trial.
So the combination of AS, stomach discomfort, my own GP wanting to check on the thyroid condition – all these led to my AML diagnosis.
Throughout the whole of this experience I am lucky not to have actually ever felt ill. This is partly a consequence of the pandemic lockdown, as a result of which I’ve not been doing anything which needed much exertion and with isolation I haven’t ‘caught’ anything.


Gerard with his granddaughter on his 80th birthday
My wife and I had our second COVID vaccination on 9th January, which is very reassuring.
My day-to-day interests have gone on as usual – the newspaper, crosswords, politics, the piano, cooking, wine, a bit of gardening, a bit of DIY. We miss the socialising we had previously, particularly wining and dining with friends.
None of the drugs or treatments have left me nauseous or in pain. I don’t like all the blood taking and the bone-marrow biopsies – but they are actually quite trivial experiences and the staff involved are all careful and caring.
Also, as I live only 10 minutes drive from The Christie I don’t need to hang around for long periods – I can go home and they will ring me when I’m needed.


Madeline Hawkins was diagnosed with Chronic Myeloid Leukaemia (CML) back in June 2012 after she was referred for additional blood tests following complains of pain in her feet.

Patient/caregiver volunteers required to support a clinical trial proposal for patients with AML